Monitoring in Sepsis and ARDS
How can technology help?
How can PiCCO help? - David Kaufman, New York, USA
Notes/Discussions
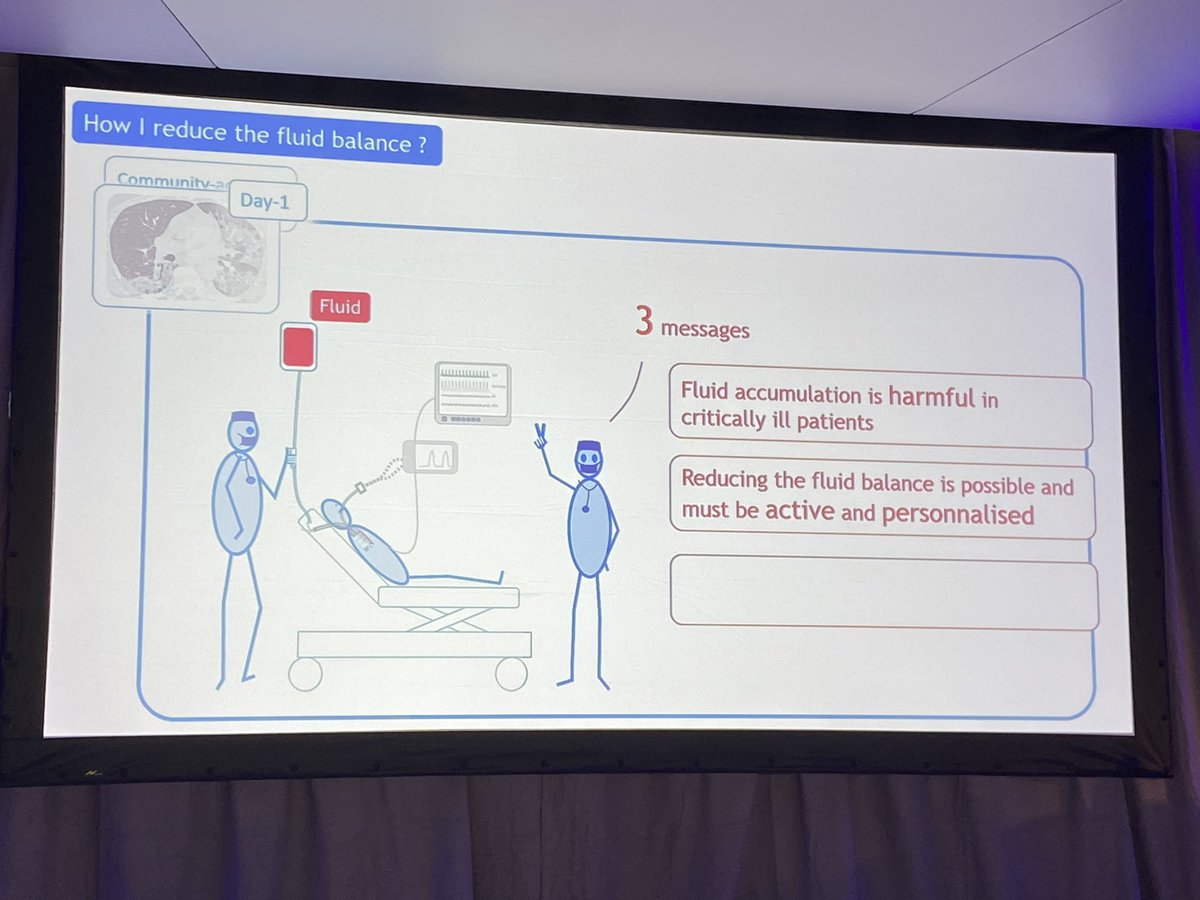
David Kaufman, from NYU School of Medicine, is Director of the Medical Intensive Care Unit. He opens his talk by telling us his objectives (thank you!): when to start fluid, stop fluid and remove fluid, and how pulse contour devices can assist.
He outlines a depressing but common case of a 22 year old man who progressed to develop fulminate multi-organ failure and dies. He suggests that this was in part due to iatrogenic fluid excess.
So why do we give fluids? We want to improve organ function, which requires increased micro-flow, which requires improved macro-flow (debatable). Macro-flow, or cardiac output, requires increased stroke volume, which requires increased venous return, which may require a bolus of fluid. David describes this considerably better using a graphic on a slide!
“The benefit of continuous cardiac output monitoring is that it gives us information about where our patient exists on the Frank-Starling curve.”
How can PCCO help?
- Identifying low cardiac output state
- Identifying when cardiac output can be improved with fluid
- Identifying the formation of lung oedema
- Identifying what your patient needs
What’s the evidence? Not great. There is one study in septic patients (the rest being peri-operative or non-English). Richard et al, Critical Care 2015; 19:5. Single centre with ~60 patients.
“Don’t pay attention to the p-value… look at the magnitude of the effect” - I totally agree with David’s point.
And finally, when a patient is on the ‘flat’ portion of the Starling curve, then we can be reassured that removal of fluid is safe to perform.
Summary/Key points
- Continuous pulse contour analysis with trans pulmonary thermodilution offers information and guidance that other strategies can’t
- Starting fluid therapy, stopping it, and then removing it can all be guided by PCCO with TPTD
- Finding the ‘sweet spot’ of our patients will reduce harm
How can the Swan help? - Thomas Scheeren, Groningen, The Netherlands
Notes/Discussions
Thomas Scheeren talks us through his thoughts on the Swan-Ganz pulmonary catheter. He starts by describing how the evidence is mixed and the utilisation has drastically reduced. Why? Insufficient clinician knowledge, evidence of no benefit or possibly harm, and alternative strategies such as pulse contour analysis or Echocardiography. So the international consensus states “We do not recommend the routine use of the pulmonary catheter (Level 1a)”.
So is the Swan dead, asks Thomas. He reminds us that it can provide cardiac output measurement as is probably the gold standard for this. Furthermore, it helps answer the question “Is the cardiac output adequate for this patient?”. Through measurement of wedge pressures, it can help answer the question, “Does the patient need fluid?”
Thomas quotes a trial from 2012 (Bethlehem, Critical Care Research and Ractice 2012) to show how a PAC can lead to more fluid early in care and a reduction in fluid balance in the later stages of care.
Summary/Key points
- The PAC provides better and unique monitoring compared to other devices
- It may provide guidance for the treatment of patients with sepsis and ARDS
How can ultrasound help? - Daniel Lichtenstein, Paris, France
Notes/Discussions
Daniel Lichtenstein opens with a big statement: “After three decades, I am still an independent researcher with no conflicts of interest.” He does go on to say he has a bias of personal opinion. Both very good personal reflections, IMO.
“I still do not know if the patient died in spite of my therapy, or because of my therapy”. A tough dilemma we all face.
Daniel talks us through his BLUE and FALLS protocols. It looks like a complex protocol on screen but from my personal experience, they are easy to follow.
The BLUE protocol identifies one of four profiles:
- B profile
- C profile
- A/B profile
- A-V-PLAPS profile
In identifying one of these, the combined specificity for pneumonia is 89%. Can any blood test achieve that?
Daniel reminds us that ARDS is not a disease, but a syndrome due to many causes (of which the majority are a types of pneumonia).
Using the FALLS protocol, we can systematically rule out causes of shock
- Pericardial tamponade
- Pulmonary embolism (with shock)
- Pneumothorax
- Obstructive shock
- Cardiogenic shock
Once these are ruled out, a fluid therapy can be initiated with confidence.
And how do we find the source of sepsis? Daniel talks us through how ultrasound can help us. If we find a pleural effusion, suspect pneumonia and tap that effusion for microbial identification. If we find pneumoperitoneum, suspect gut trouble and call a surgeon. Daniel goes on to talk us through abdominal and gut ultrasound, with some advanced techniques. He also shows us an amazing ultrasound loop of a floating venous thrombus.
Summary/Key points
- Use your usual tools at the bed side, and add ultrasound to these
- Use BLUE to guide diagnosis in the patient with respiratory failure
- Await further research before using FALLS to guide fluid therapy in shocked patients
References
- https://t.co/TkwTy6q8b1 The BLUE protocol
How can dynamic imaging help? - Daniel Reuter, Rostock, Germany
Notes/Discussions
Daniel Reuter talks us through strategies to monitor our patients. He shows us some pretty pictures of false-colour CT scans of pig lungs to demonstrate the high hetrogeneity of lungs in ARDS.
Next up, he talks us through bioimpedance techniques to give realtime dynamic imaging of the lungs. Looks great but difficult to implement and full of limitations. “We used superglue to get best contact in our animal models.” More pretty pictures demonstrate how the Open Lung Approach may lead to better ventilation than the classic ARDSnet strategy, as demonstrated in real time by impedance tomography.